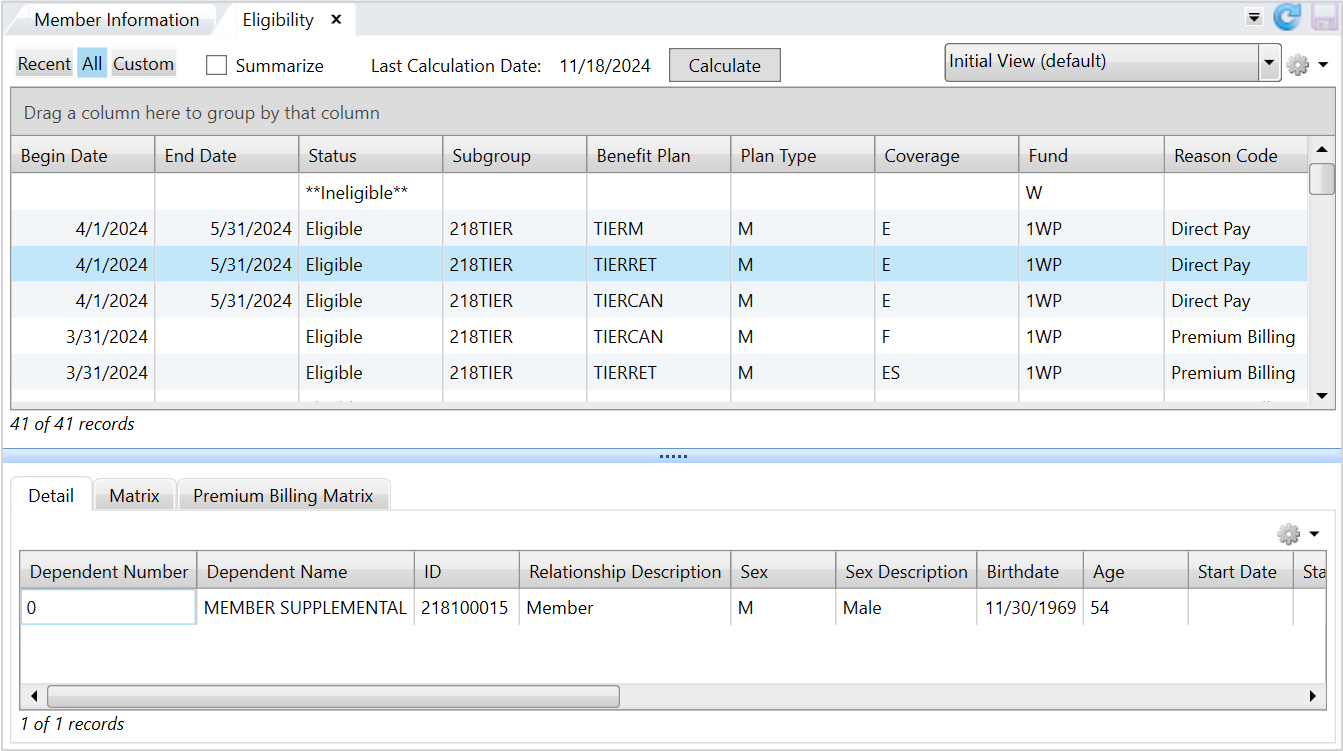
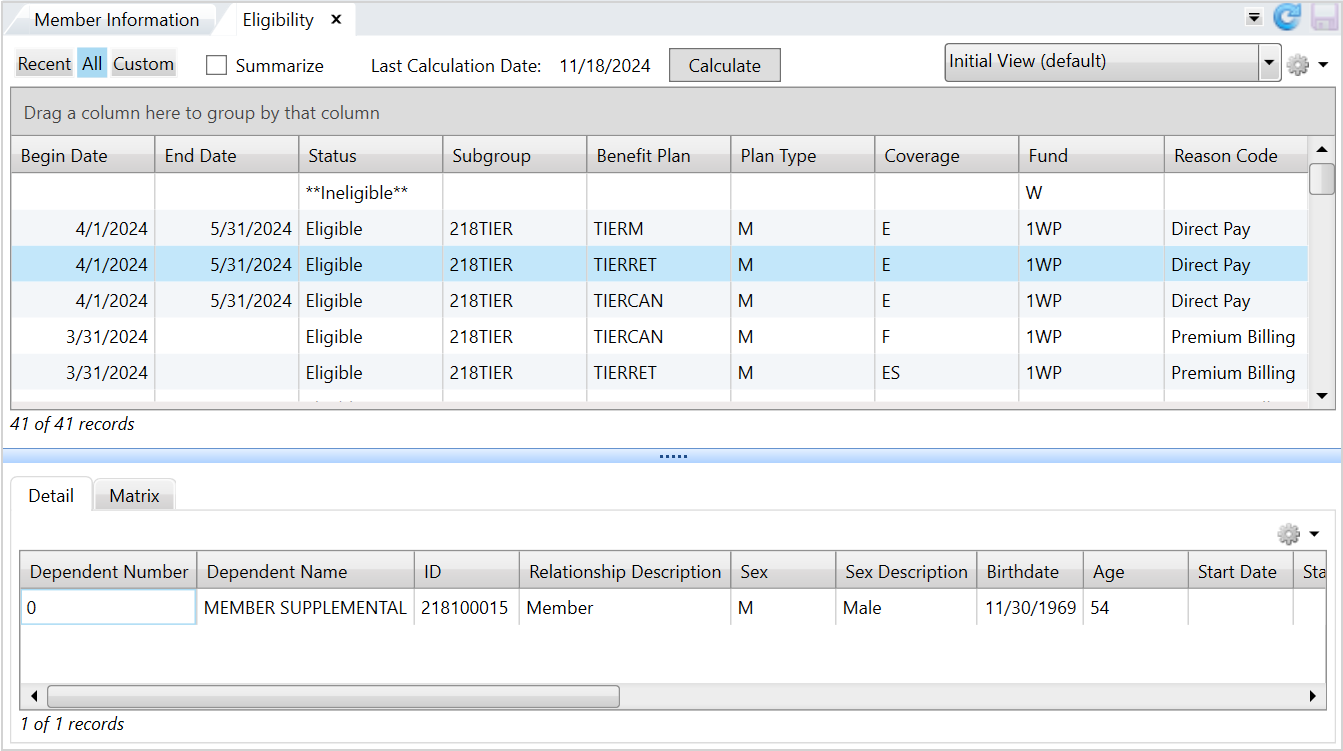
Eligibility
The Eligibility tab displays complete eligibility information so you can answer inquiries from members concerning their eligibility for benefits, (medical,
Eligibility information bar
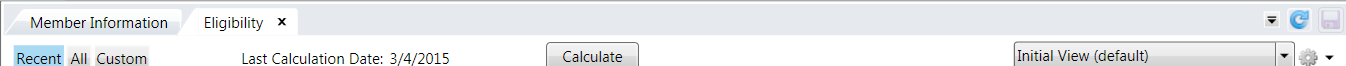
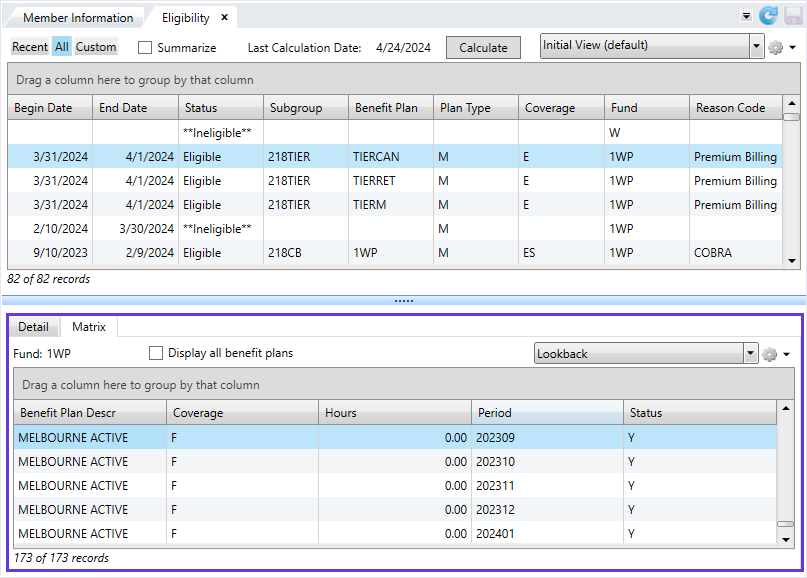
From the Eligibility information bar, view the individual's most recent eligibility, eligibility history, or custom eligibility (based on your system setup).
- Choose the most recent eligibility, eligibility history, or custom eligibility date with the
Recent,All, andCustomfilters, at the top of theEligibilitytab. The results display in theEligibilitytable. - Select the
Summarizecheck box to switch between a summarized eligibility view and a detailed view. The summarized view combines multiple rows of data in theBenefit Plan,Benefit Plan Name,Plan Type,Plan Type Name,Coverage, andCoverage Namecolumns to one row. - The last date the individual's eligibility was calculated displays here and you can recalculate the eligibility with the
Calculatebutton. See the Filter to display the individual's most recent eligibility data. .
<87> Auto calculate eligibility when opening a member. When set to Y, the member's eligibility recalculates when opening in ServiceXG. If N or blank (the default), it won't recalculate on opening.Eligibility table
The Eligibility table displays the individual's most recent eligibility, eligibility history, or custom eligibility date (based on your system setup).
| Field | Description |
|---|---|
| Agent |
Person or entity that represents the member for benefit coverage. |
| Begin Date |
Date the eligibility coverage began. |
| Benefit Plan |
Benefit plan code associated with the eligibility period. The benefit plan identifies the benefits an individual receives as the result of the individual's association with a subgroup. If you selected the |
| Benefit Plan Name |
Name of the benefit plan. If you selected the |
| Billing Account | The billing account associated with the member. |
| Country | Individual's country. |
| Coverage |
Coverage code for the eligibility period. The coverage code identifies who is covered by a benefit plan type, for example, individual or family. If you selected the |
| Coverage Name |
Name/description of the coverage code. If you selected the |
| Dependent | A dependent number identifies the member and dependents covered by the benefit plan, for example, 0 refers to the member. Dependent numbers 1 and above refer to specific dependents and the dependent number was assigned when the dependent was entered in the system. |
| Employer |
Sponsoring employer's ID. |
| Employer Name |
Name of the sponsoring employer. Note: If the fund is a multi-employer fund, this field will display as |
| End Date |
Date the eligibility ended (terminated). If there is no end date, the benefit doesn't terminate. |
| End Date Reason | Description of why the coverage was terminated. |
| End Date Cd | Code indicating why the coverage was terminated. |
| Fund | Fund code associated with the contribution or payment. A fund is a legal entity for the contributions and distributions of money. |
| Fund Name |
Name of the fund associated with the contribution or payment. A fund is a legal entity for the contributions and distributions of money. |
| Network |
Network code associated with eligibility in an HMO environment. Note: This data is only available if you have a modified tape load function that allows you to load this data. |
| Option | The option for the benefit plan associated with the member. |
| PCP |
Primary Care Physician (PCP Note: This data is only available if you have a modified tape load function that allows for you to load this data . |
| Plan Type |
Plan type code associated with the individual. A plan type identifies a type of benefit plan, such as medical, dental or vision. |
| Plan Type Name |
Name/description of the plan type such as medical, dental, or vision. |
| Reason Code |
Reason that eligibility started or ended.
|
| Site |
Code associated with the Primary Care Provider (PCP) in a Health Management Organization (HMO). Note: This data is only available if you have a modified tape load function that allows you to load this data. |
| Status |
Individual's eligibility status:
|
| Subgroup |
User-defined code representing a grouping of benefits associated with the individual's eligibility. |
| Subgroup Name | Name of the subgroup. |
You can switch between the most recent eligibility, eligibility history, or custom eligibility with the Recent, All, and Custom filter options at the top left of the Eligibility tab.
The Eligibility table is read-only so you can't add, update, or delete the information, but you can sort, filter, and group data, and create and save a different view![]() A custom-defined representation of the data. of the data that display. Refer to Common features (for standard table features) and Views for details.
A custom-defined representation of the data. of the data that display. Refer to Common features (for standard table features) and Views for details.
Below the Eligibility table is an expandable and collapsible panel that displays the Detail tab and the Matrix tab. These tabs display more details about the selected row of eligibility information.
Detail tab
| Field | Description |
|---|---|
| Dependent Number |
A dependent number identifies the member and dependents covered by the benefit plan, for example, 0 refers to the member. Dependent numbers 1 and above refer to specific dependents and the dependent number was assigned when the dependent was entered in the system. |
| Dependent Name |
Name of the individual. |
| ID |
Individual's Social Security Number. |
| Relation Description |
Relationship to the member, for example, member, spouse or dependent. |
| Sex Description |
Individual's sex (male, female or unknown). |
| Birth date |
Individual's birth date. |
| Age |
Individual's current age. |
| Start Date |
Individual's most current start date with the membership. Note: The dependent can't have eligibility before this date. |
| Start Reason Description | Status code associated with the start date |
| Term Date | Termination date for individual's benefit plan. |
| Term Reason Description | Textual description of reason for termination of eligibility. |
| Medicare Type |
Code that identifies the type of medicare coverage. |
| Medicare Type Description |
The reason the individual is eligible for Medicare coverage: |
| Medicare Effective | Date the individual is eligible for Medicare. |
| Medicare Expiration | Last date of the individual's Medicare coverage. |
| Sex | Code that indicates the individual's sex. |
| Relation | Code that indicates the individual's relationship to the member. |
| Start Reason | Code for reason coverage was begun. |
| Term Reason | Code for reason coverage was terminated. |
The Detail tab table is read-only. You can't add, update, or delete the eligibility information. Also, you can't choose the data that displays in the table, but you can perform some standard table functions like moving columns around, and sorting and printing the data. To print or export the data from the table, click ![]() and select the appropriate option. See Common features for more information on printing and exporting data from a table.
and select the appropriate option. See Common features for more information on printing and exporting data from a table.
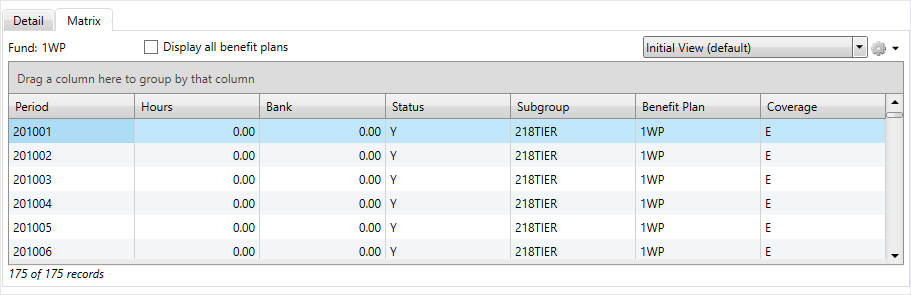
Matrix tab
The Matrix table displays the eligibility being calculated and includes the rules, work period, and other details. The matrix header contains the Fund and Display all benefit plans check box. The Fund displays for the selected member's eligibility. If the member is ineligible, no fund displays. The Display all benefit plans check box lets you view all benefit plans.
The monthly eligibility information can help you troubleshoot or respond to discrepancies in a member's eligibility. For example, you might have calculated that a member should have eligibility through December, but the record only shows eligibility through November. You can walk through the eligibility month-by-month to check for discrepancies.
| Field | Description |
|---|---|
| Display all benefit plans | Displays matrix tab information for the individual’s benefit plans. |
| Accum Hrs Self-Pay | Accumulated self-pay hours. Individuals who have insufficient hours worked for contributions pay an amount (self-pay) to retain eligibility. Depending on the plan, this amount can be a flat rate or a base rate that is multiplied by the number of hours needed. |
| Bank | Number of hours/dollars banked (if the eligibility rules allow for banking of hours or dollars in excess of the required hours/dollars). These hours/dollars can be used later to obtain eligibility. |
| Benefit Plan | Benefit plan code associated with the period. The benefit plan code identifies a specific set of benefits packaged together. |
| Benefit Plan Description |
Description of the benefit plan code. |
| Benefit Plan Type | Benefit play type associated with the individual's eligibility. |
| Contract Type | Contract code. |
| Contribution Rate | Rate used to calculate the individual's contributions. |
| Coverage | Coverage code associated with the period. The coverage code identifies who is covered by the benefit plan, for example, individual or family. |
| Coverage Desc | Description of the coverage code. |
| Criteria Type | Criteria used in the eligibility schedule |
| Criteria Dol |
Dollar amount by criteria type used in the eligibility schedule. |
| Criteria Hrs |
Number of hours by criteria type used in the eligibility schedule. |
| Dollars | Total dollar amount contributed on behalf of the member for the fund, for the work period. This amount is the rate multiplied by the quantity. |
| Excess Bank | Number of hours/dollars over the maximum number of hours/dollars banked. |
| Hour Non Re-Use | Hours which have been marked for non re-use. |
| Hours | Number of hours reported for the fund, for the period. |
| Hours-No Self Hrs | Quantity of hours exceeding any self-pay quantity; typically refers to hours but can be days or wages. |
| Period |
Period in which contributions are posted and eligibility is given according to the rules of the fund which are defined in the eligibility schedule. When examining contributions in the eligibility matrix, this is the work period. When examining the eligibility status, this is considered the eligibility period. |
| Self-Pay Cnt | Amount the individual can self pay to become eligible for benefits. |
| Self-Pay Due | Amount of self pay dollars due. This is the self pay contributions minus the self pay amount paid. |
| Self-Pay Paid | Amount of self-pay money paid to maintain coverage. |
| Self-Pay Part Rfnd | Amount of a partial refund of self-pay money. This will occur if different rules are used to buy eligibility in different months within the same period (eligibility period). |
| Self-Pay Amount | Contribution amount paid by the individual to obtain eligibility. |
| Self-Pay Refund | Self-pay refund amount. |
| Status |
Eligibility status for the period (the period when looking at the status is the eligibility period.) If a Y is in the first position, the individual is eligible for the benefit aligned with this status and period; any other character designates ineligibility. |
| Subgroup | User-defined code representing a benefit grouping associated with the individual's eligibility for the benefit period’s plan and coverage. |
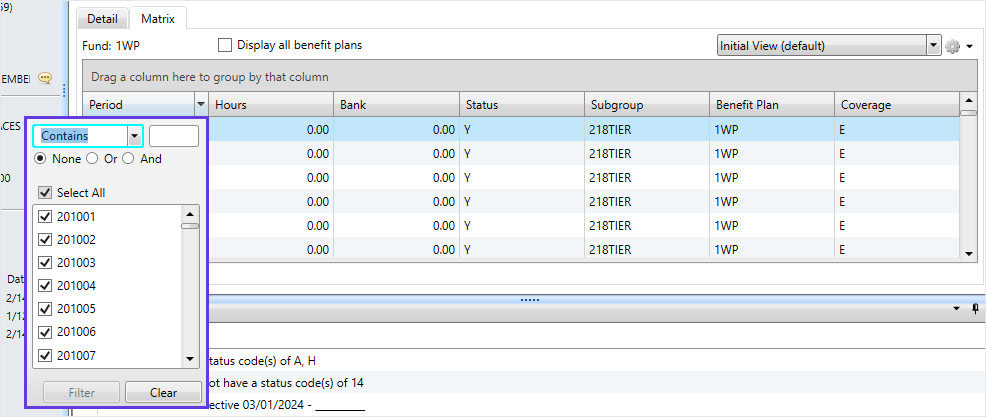
The Matrix table is read-only so you can't add, update, or delete the eligibility information but, you can choose the data that displays as well as sort, filter, and group data, and create and save a different data view. Refer to the Common features (for standard table features) and Views topics for more details.
For example, the matrix displays all historical work periods with the earliest at the top, but you can use the filter to view more recent work periods.
You can apply filters to specific columns by selecting the dropdown arrow  . Filters can: Contain, Equal, Not Equal, Start with, or End with alphanumeric data.
Be Equal, Not Equal, Greater, or Less than a selected Received date.
Apply additional operators such as
. Filters can: Contain, Equal, Not Equal, Start with, or End with alphanumeric data.
Be Equal, Not Equal, Greater, or Less than a selected Received date.
Apply additional operators such as Or and And for more refinement.
Select the filter  and choose the information to filter by. For example, select
and choose the information to filter by. For example, select  and choose the work periods to include or exclude.
and choose the work periods to include or exclude.
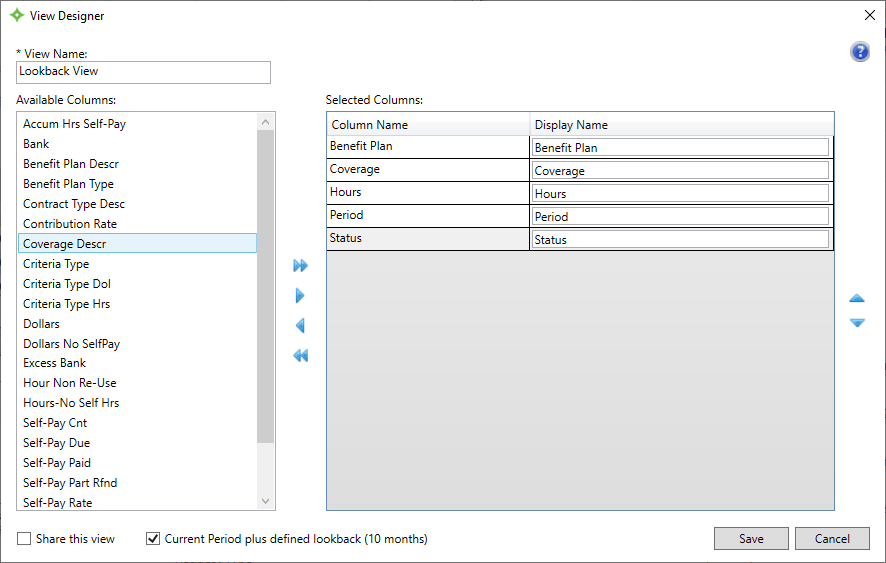
Matrix View Designer
The eligibility matrix contains a view designer that lets you control which work periods display in the beginning of the table. You can either view a member's first eligible work period or the current period plus a defined number of lookback periods.
ELG SAC <103> - ELG Matrix Display Period Lookback. This SAC defines the number of work periods to look back when the eligibility matrix view designer is configured to use the Current Period plus lookback. Contact your administrator for more information.For example, the default setting is to view the historical work periods. If the member's eligibility dates back to October 2002, the work period for 200210 would display first in the matrix.
However, from the view designer, you can change this setting to display the current work period and a specified number of lookback work periods. If the current period is July 2024 (202407), and you set the ELG Matrix Display Period Lookback SAC to 10, the matrix would set the focus of the display to the 10th month prior to the current July work period. All work periods remain in the display you can scroll as needed to review other periods.
- Select
 from the
from the Matrixtab. - Click
Add vieworEdit view. - From the
View Designerwindow, select theCurrent Period plus defined lookback (X months)check box to have the matrix table display the current period plus the defined lookback. In this example, the lookback was set to 10 months. - Finish editing your view and click
 to save.
to save. - The
Matrixtable now displays the current period plus the lookback months. If a member doesn't have enough history to display the number of lookback months, the table displays as much information as possible. - To return to viewing the member's first period, open the
View Designerand deselectCurrent Period plus defined lookback.
Premium Billing Matrix tab
On the Premium Billing Matrix tab, you can view member eligibility calculations and their employment status changes.
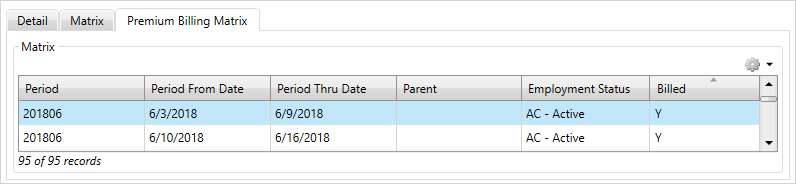
| Field | Description |
|---|---|
| Period | The current billing period. |
| Period From | The period from date. |
| Period Thru | The period thru date. |
| Parent | Indicates if there's an associated parent employment status for the period. |
| Employment Status | The member's employment status for the period. |
| Billed |
Indicates if the period was billed.
|
The Premium Billing Matrix tab is read-only. You can't add, update, or delete the eligibility information, but you can sort and filter the information that displays. Refer to the Common features topic for standard table features and the topic to change the data columns in the view![]() A custom-defined representation of the data..
A custom-defined representation of the data..
To print or export the data from the table, click ![]() and select the appropriate option. See Common features for more information on printing and exporting data from a table.
and select the appropriate option. See Common features for more information on printing and exporting data from a table.